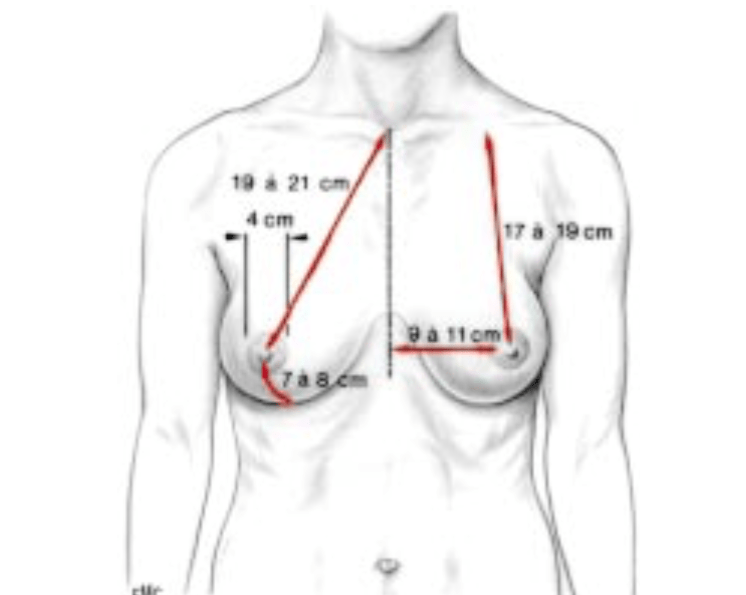
Ideal anatomy and proportion:
The ideal breast is 10-12 cm wide and the 2 nipples, centered in the middle of the breast, are about 20 cm apart (variable according to thorax width and patient morphology). The areola, with an ideal diameter of 38-45 mm, should be located 20 cm from the top of the sternum or halfway between the shoulder (acromion) and the elbow (epicondyle) and the distance between the nipple and the submammary fold should be about 7 cm.
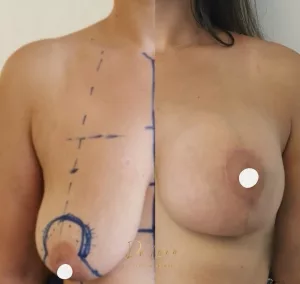
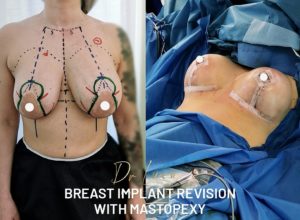
Over time, after a change in weight, pregnancy or breastfeeding, the breast tends to sag (ptosis) and the cleavage becomes empty. Mastopexy prosthesis surgery allows the breast to be lifted, while filling the cleavage.
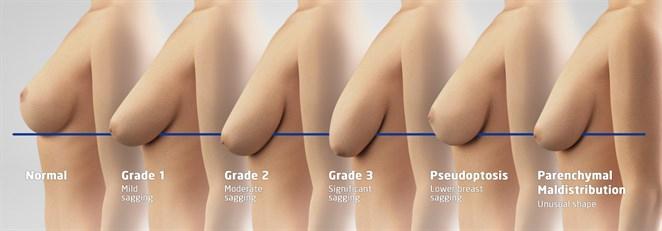
The areola should ideally be at the height of half the arm or 2-3 cm above the submammary fold (Pitanguy’s point) and most of the breast volume should be above the horizontal line corresponding to the submammary fold:
- If the nipple is at the level of the submammary fold, it is called type I (minimal) ptosis
- If the nipple is 1 to 3 cm below the submammary fold, it is called type II ptosis (moderate)
- If the nipple is more than 3 cm below the submammary fold, it is called type III ptosis (severe)
Technique
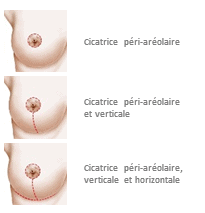
In grade II and III ptosis, a breast lift with inverted T scars is essential. In grade I, a breast lift with a periareolar scar (around the areola) and sometimes a vertical scar only can be performed.
The procedure is performed under general anesthesia. Dr. Lucas, who was trained at the breast center of the CHUV (University Hospital of Lausanne), performs a scar starting around the nipples but hidden in the colored part of the areola, extending vertically from the nipple to the submammary fold, then in grade II and III ptosis, horizontally hidden in the submammary fold. Creation of a pocket, usually behind the muscle, whose dimensions are adapted to the projection and diameter of the implant. Partial disinsertion of the pectoral muscle fibers on the sternum to create a natural cleavage.
The glandular breast tissue is preserved as much as possible, unlike breast reductions, and then a skin closure is performed. Dr. Lucas reshapes the structure of the mammary gland to fill the cleavage and restore volume in the upper breast.
Dr. Lucas uses biological surgical glue for the scar so that the patient can shower on the second day after the procedure. In general, the procedure is performed on an outpatient basis, without the need for hospitalization.
Results:
Time to final results:
2 weeks to see a significant result, 2 to 5 months to see the final result
Longevity of results:
Definitive, but with weight changes, pregnancies, breastfeeding and time the breast will evolve.
Before surgery:
Stop smoking 1 month before surgery (risk of necrosis of the areola important if active smoking)
Do not take Aspirin 10 days before the operation, inform Dr. Lucas of any anticoagulant medication (Sintrom, Coumadin, Eliquis, etc.) in order to arrange for its discontinuation or replacement.
Shower with Hibiscrub soap provided on the prescription 48 hours before
No shaving of the axillary zone in the 48 hours before the operation
For patients over 35 years of age or if there is a family history of breast cancer, a screening mammogram should ideally be performed.
On the day of the procedure, you must fast for 6 hours beforehand (do not drink, eat or smoke).
Purchase before the procedure by you of a postoperative bra, the size of which will be specified to you by Dr. Lucas or a girdle, if lipofilling.
Procedure :
Duration of procedure: 120-180 minutes
Anesthesia: general
Location: operating room
Outpatient: no hospitalization, no redons
After surgery:
Post-operative pain: 2 to 4/10 the first week, with analgesia by Dafalgan, Irfen and Tramal then after the 1st week, pain at 1/10: painkillers can be gradually stopped. Post-operative pain is significantly reduced because Dr. Lucas performs a pectoral nerve block with a long-acting anesthetic during the operation.
Social eviction: 4-7 days with some discomfort. Shower possible from the 2nd day thanks to the use by Dr Lucas of biological surgical glue replacing the dressings.
Return to work: 7 days
Resumption of sports: 6-8 weeks
Instructions:
Permanent cessation of smoking to minimize complications, mandatory if lipofilling
Control Dr Lucas D2, D7, 3 weeks, 3 months, 6 months, 1 year
During the first 3 days especially: no rapid effort, rest, do not get up too quickly, take it easy so as not to make any sudden movements (efforts may increase the tension and open the small vessels and thus cause a hematoma)
Compression bandage around the breasts for 24-48 hours, then put in place during the consultation at 2 days of the support bra
Do not lift your arms above 100°, do not carry heavy loads > 3-4 kg and do not push for 6 weeks: the body will form a capsule around the implant during these first 6 weeks, this capsule will accompany you throughout your life. It is essential to respect these instructions during the first six weeks, so that it forms in good conditions.
Bra without underwire 3 weeks day and night, 3 weeks during the day.
Shower from the 2nd day: pass water over the scar without rubbing, dab with clean cloth without rubbing
Between the 2nd day and the 7th day, disinfect the wound once a day with Merfen spray or another disinfectant spray.
From the 15th day, gently rub glue on the scar which will disappear over several days without tearing it off
Bath from 3 weeks depending on the evolution of the scar at 3 weeks.
Massage scar with Gorgonium 2 times 5 minutes per day for 3 months after the shower, from the 15th day.
Strataderm silicone once a day for 3 months, starting on the 15th day.
Sun protection with an index higher than 50 during the 6 months following the surgery.
Follow-up of the scar by Dr. Lucas for 1 year after the surgery is essential.
Complications
– Hematoma, seroma: a hematoma can occur especially during the first 48 hours. If it is significant, it is necessary to intervene again and evacuate it. During the first few days, it is necessary to rest and not to make any sudden movements in order to reduce the risk of hematoma.
– Localized skin necrosis, necrosis of the areola: the risk of this is greatly increased by smoking intoxication.
– Infection: fortunately rare, infection may require antibiotic treatment and a new surgical intervention to remove the implants. These can only be put back in place after several months of healing.
– Decreased sensitivity of the areola: often transient, full recovery is generally achieved after a few months.
– Asymmetry
– Rippling (folding of the prosthesis) or feeling of the prosthesis laterally: can be seen in thin patients or after significant weight loss: often transient, but if it remains after 6 months, it can be corrected by lipofilling (fat transfer).
– Abnormal, hypertrophic or even keloid scars: patients with dark skin, at risk of abnormal scars, must pay particular attention to scar care with Gorgonium and Strataderm, follow-up remains essential
– Rupture: rare, often after several decades, rupture requires a change of the implant
– Malposition of the implant: rare, but requires a re-intervention.
– Capsulitis: the capsule formed around the implant follows you throughout your life, until (often after 10-20 years) it becomes inflamed and causes capsulitis. This manifests itself as pain, initially with effort, which gradually sets in at rest. Then, the breast loses its flexibility and in cases of advanced capsulitis, the breast is deformed. When the patient presents pain and the capsulitis is confirmed by imaging (ultrasound or MRI), the implant must be changed and the capsule removed (capsulectomy).
– Breast implants and breastfeeding: there is no consequence on breastfeeding, the patient can breastfeed after a breast augmentation by prosthesis.
– Scar dehiscence and delayed healing (favored by smoking): sometimes there are small openings of the scar of a few millimeters, which can be treated with dressings usually without the need for reoperation. The follow-up by Dr. Lucas of the scar is essential.
Combinations and alternatives
A abdominoplasty can be combined in the same operation time to perform what is called “Mommy makeover”: breast lift, breast implant associated with an abdominoplasty.